Cell-based Gene Therapy Treatment Cures Hemophilia B in Model
By LabMedica International staff writers
Posted on 17 May 2018
A novel, cell-based gene therapy approach was used to cure hemophilia B in a mouse model of the disease.Posted on 17 May 2018
Hemophilia B, a blood-clotting disorder caused by defects in the gene encoding the protein-clotting factor IX (FIX) is considered to be an appropriate target for gene- and cell-based therapies due to its monogenic nature and broad therapeutic index.
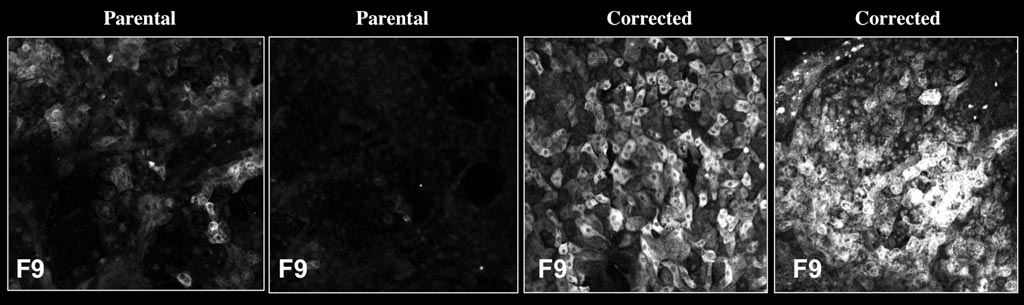
Image: Left two panels: Hepatocyte-like cells (HLCs) differentiated from the stem cells of patients with hemophilia B show very low levels of clotting factor IX, (FIX), shown in white. Right two panels: After treating these same cell lines with a gene correction tool, FIX increased to healthy levels (Photo courtesy of the Salk Institute).
Toward this end, investigators at the Salk Institute (La Jolla, CA, USA) used their FIX-deficient mouse model to evaluate the use of cell therapy as a potential long-term cure for hemophilia B. Initially, they showed that transplanted, cryopreserved, cadaveric human hepatocytes remained functional for more than a year and secreted FIX at therapeutic levels. Hepatocytes from different sources (companies and donors) performed comparably in curing the bleeding defect.
Next, the investigators generated induced pluripotent stem cells (iPSCs) from two hemophilia B patients and used the CRISPR/Cas9 gene-editing tool to correct the disease-causing mutations. These corrected iPSCs were coaxed into differentiating into hepatocyte-like cells (HLCs) and were then transplanted into hemophilic mice.
Results published in the May 1, 2018, online edition of the journal Cell Reports revealed that the transplanted iPSC-HLCs produced enough FIX to enable the mice to form normal blood clots, and that the cells continued to survive and produce FIX for at least nine to 12 months.
"The appeal of a cell-based approach is that you minimize the number of treatments that a patient needs," said first author Dr. Suvasini Ramaswamy, a former research associate at the Salk Institute. "Rather than constant injections, you can do this in one shot."
Related Links:
Salk Institute













