Depressing Stress Signaling Increases Immune Activity
By LabMedica International staff writers
Posted on 12 Sep 2017
Cancer researchers evaluating the immune status of the tumor microenvironment found that CD8+ T-cell frequency and functional orientation were regulated by beta-2-adrenergic receptor (beta-AR) signaling and suggested using clinically available beta-blockers in patients to improve responses to immunotherapy.Posted on 12 Sep 2017
Anticancer therapies designed to block “checkpoints” within the immune system do not work for all patients, and their efficacy in controlling tumors is often short-lived. To better understand these phenomena and to improve the performance of check point inhibitors, investigators at Roswell Park Cancer Institute (Buffalo, NY, USA) used three strategies: physiologic (manipulation of ambient thermal environment), pharmacologic (beta-blockers), and genetic (beta-2-adrenergic receptor knockout mice) to reduce adrenergic stress signaling in two widely studied preclinical mouse tumor models.
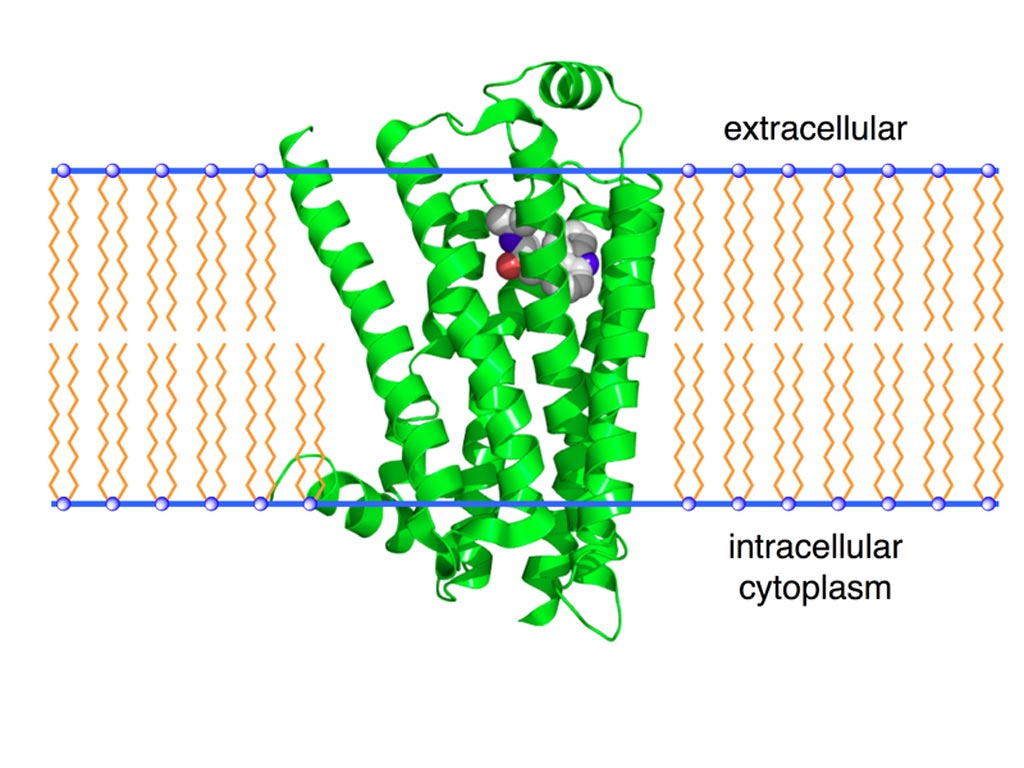
Image: A ribbon model of the beta-2 adrenergic receptor (Photo courtesy of Wikimedia Commons).
They reported in the August 17, 2017, online edition of the journal Cancer Research that reducing beta-AR signaling facilitated conversion of tumors to an immunologically active tumor microenvironment. This immunologically enriched microenvironment displayed increased frequency of CD8+ T-cells with an effector phenotype and decreased expression of PD-1, in addition to an elevated effector CD8+ T-cell to CD4+ regulatory T-cell ratio. Moreover, this conversion significantly increased the efficacy of anti-PD-1 checkpoint blockade.
In short, manipulating beta-adrenergic receptor signaling to regulate the immune status of the tumor microenvironment supported the strategic use of clinically available beta-blockers in patients to improve responses to immunotherapy.
“Our bodies respond to certain types of stress - such as fear and anxiety, heat, cold, pain, depression, and even attack by cancer cells - in the same way. We jump into "fight or flight" mode, and the sympathetic nervous system dials up the release of norepinephrine,” said senior author Dr. Elizabeth Repasky, professor of immunology at Roswell Park Cancer Institute. “For reasons that we do not entirely understand yet, prolonged exposure to these stressors often makes our immune cells much less effective. But we demonstrate here that beta blockers, by reducing adrenergic signaling, allow anti-tumor immune cells to become much stronger, and give immunotherapies, and in particular checkpoint inhibitors, a much better chance to work.”
Related Links:
Roswell Park Cancer Institute













