Staphylococcus Aureus Avoids Inducing Immune Memory in Model
By LabMedica International staff writers
Posted on 03 Oct 2017
A team of medical microbiologists has identified the mechanism that prevents the body's immune system from developing an effective protective response to repeated Staphylococcus aureus infections.Posted on 03 Oct 2017
Investigators at Cedars-Sinai Medical Center (Los Angeles, CA, USA) sought to clarify why humans do not usually develop effective immunity to Staphylococcus aureus reinfection.
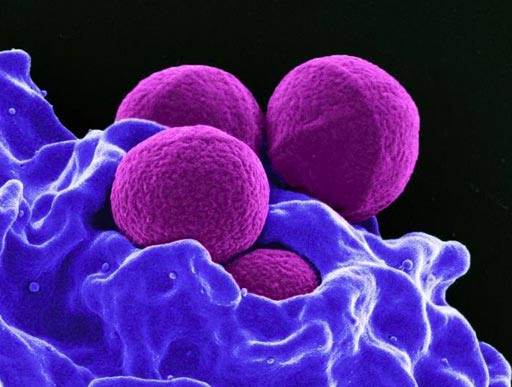
Image: Four spherical S. aureus bacteria being enveloped and destroyed by human white blood cells (Photo courtesy of the U.S. National Institute of Allergy and Infectious Diseases).
Toward this end, the investigators worked with a mouse model that mimicked human S. aureus infection. They reported in the September 21, 2017, online edition of the journal Cell Host & Microbe that infection by S. aureus caused the immune system to increase production of anti-inflammatory cytokines, specifically interleukin-10 (IL-10), while impairing the anti-pathogenic response from protective Th17 (T helper) cells.
At the mechanistic level they found that O-acetylation of peptidoglycan, a mechanism utilized by S. aureus to block bacterial cell wall breakdown, limited the induction of pro-inflammatory signals required for optimal Th17 polarization. Thus, the bacterial cell wall remained intact after infecting the host, and molecules from the pathogen did not escape to interact with the immune system and trigger the development of robust protective immune memory.
IL-10 deficiency in mice restored protective immunity to S. aureus infection. Using a staphylococcal peptidoglycan O-acetyltransferase mutant as adjuvant reduced IL-10, increased IL-1beta (an important mediator of the inflammatory response), and promoted development of IL-17-dependent, Th cell-transferable protective immunity.
"Essentially, staph tricks the body's T-cells, which are white blood cells that fight infection, and prevents them from mounting an effective defense," said contributing author Dr. Gislaine Martins, assistant professor of biomedical science and medicine at Cedars-Sinai Medical Center. "The study explains why our immune system is fooled by staph. Staph evolved to have this enzyme that makes this modification in its cell wall. This modification protects the wall from degradation and therefore from being properly detected by the immune system, which will not remember the bacteria the next time the body is infected."
Related Links:
Cedars-Sinai Medical Center













