3D Heart Tissue Improves Drug Screening
By LabMedica International staff writers
Posted on 13 Jul 2017
Researchers have engineered a functional 3-dimensional cardiac tissue from human stem cells to better test the safety and efficacy of new drugs on the human heart.Posted on 13 Jul 2017
Currently a main part of the problem is the use of animals or animal-derived cells in preclinical cardiotoxicity studies. Substantial genetic and cardiac differences exist between animals and humans. There have been a large number of cases whereby the tests failed to detect cardiovascular toxicity when moving from animal studies to human clinical trials (>20% of drug attrition has been attributed to cardiovascular toxicity, according to Laverty et al, 2011).
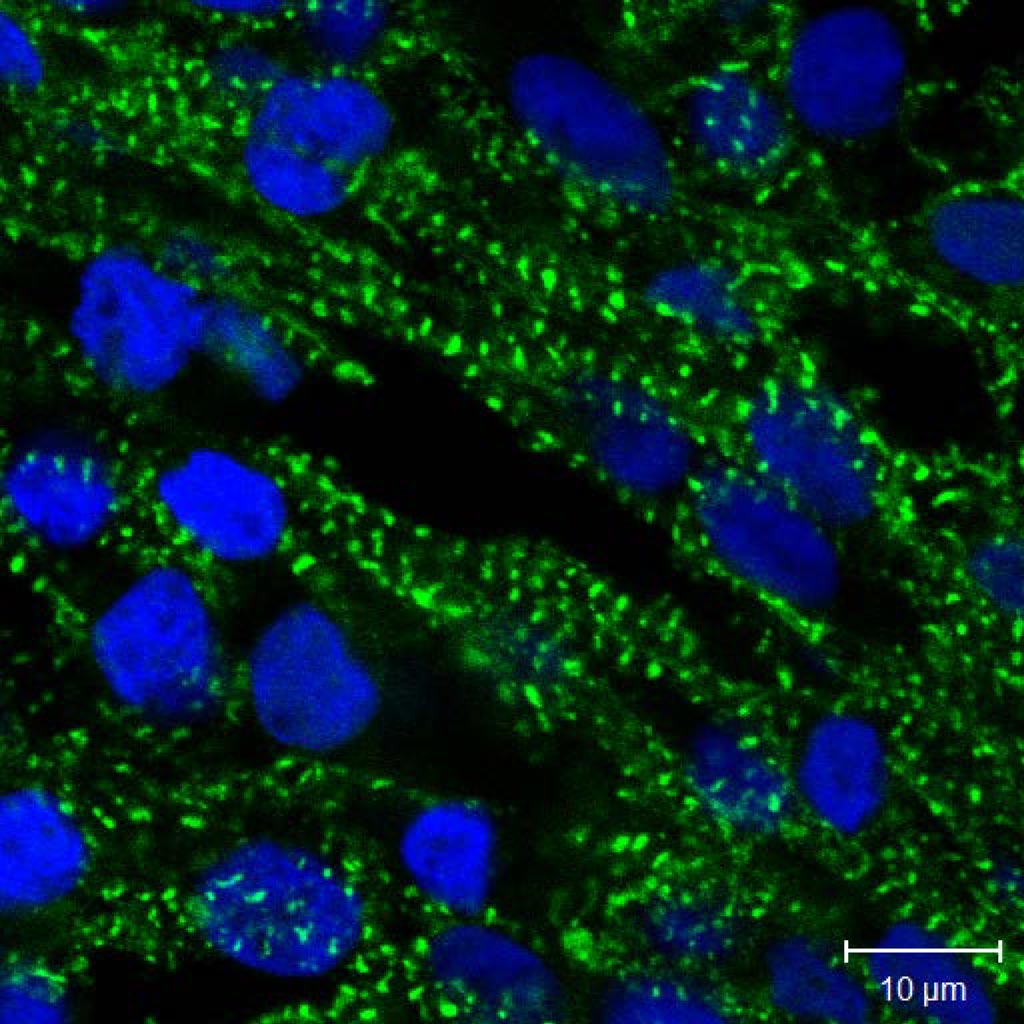
Image: Human heart muscle cells growing in the 3D tissue structure. The cells have been stained with fluorescent molecules to identify the nuclei (blue) and cardiac-specific protein (green) (Photo courtesy of IBN at A*STAR).
Existing screening methods based on 2D cardiac structure cannot accurately predict drug toxicity, while the currently available 3D structures for screening are difficult to fabricate in the quantities needed for commercial application.
To solve this problem, a research team from the Institute of Bioengineering and Nanotechnology (IBN) at A*STAR (Singapore) fabricated their 3D heart tissue from cellular self-assembly of heart muscle cells grown from human induced pluripotent stem cells. They also developed a fluorescence labeling technology to monitor changes in beating rate using a real-time video recording system. The new heart tissue exhibited more cardiac-specific genes, stronger contraction, and higher beating rate compared to cells in a 2D structure.
“Cardiotoxicity, which can lead to heart failure and even death, is a major cause of drug withdrawal from the market. Antibiotics, anticancer, and antidiabetic medications can have unanticipated side effects for the heart. So it is important to test as early as possible whether a newly developed drug is safe for human use. However, cardiotoxicity is difficult to predict in the early stages of drug development,” said Professor Jackie Y. Ying, executive director at IBN.
“Using the 3D heart tissue, we were able to correctly predict cardiotoxic effects based on changes in the beating rate, even when these were not detected by conventional tests. The method is simple and suitable for large-scale assessment of drug side effects. It could also be used to design personalized therapy using a patient’s own cells,” said lead researcher Dr Andrew Wan, team leader and principal research scientist at IBN.
The researchers have filed a patent on their human heart tissue model, and hope to work with clinicians and pharmaceutical companies to bring this technology to market.
The study, by Lu HF et al, May 11, 2017, in the journal Biofabrication.
Related Links:
Institute of Bioengineering and Nanotechnology













